Blue light therapy has become a remarkable treatment option for skin cancer patients, showing impressive clinical success rates. This innovative approach, which doctors use as part of photodynamic therapy (PDT), matches the effectiveness of surgery or radiation therapy for certain types of cancers and precancers. Research shows approximately 10% of precancerous lesions develop into squamous cell carcinoma if left untreated. Early treatment plays a vital role in prevention.
Blue Light Therapy for Skin Cancer Overview
The treatment process starts with a dermatologist applying a photosensitizing medication to the affected skin area. The blue light then activates this medication and destroys the cancerous or precancerous cells that absorbed it. The results appear promising, especially when you have clearance rates reaching 98%, which slightly edges out red light therapy’s 93% success rate.
Blue light therapy helps treat and minimize precancerous lesions called actinic keratoses, which reduces the risk of developing full-blown skin cancers. Patients usually need two or three treatment sessions to get optimal results. These sessions happen four to six weeks apart. In this piece, we’ll get into how this groundbreaking treatment works, look at the clinical evidence supporting its effectiveness, and compare it with other skin cancer treatment options.
Understanding Blue Light Therapy in Dermatology
Image Source: Newport Beach Dermatology
Blue light’s healing properties in dermatology come from its wavelength range of 407 to 420 nanometers. Blue light provides treatment benefits without causing skin aging and cancer risks that come with long-term UV exposure.
What does blue light therapy do to skin cells?
Blue light works with skin cells through several biological pathways. The light affects mitochondrial function at the cellular level by connecting with cytochrome c oxidase (complex IV of the electron transport chain). On top of that, it triggers reactive oxygen species (ROS) production in skin cells, which leads to increased oxidative stress. This process is a vital part of reducing keratinocyte proliferation after about 15 minutes of irradiation.
Blue light’s anti-inflammatory properties come from its power to increase Nrf2 expression, which blocks NF-kB—a regulator of pro-inflammatory responses. This reduces dendritic cell activation and lowers their effect on cytokine secretion by T cells. These mechanisms help explain why blue light therapy shows promise for treating inflammatory skin conditions.
The light also interacts with opsin photoreceptors (OPN2, OPN3, and OPN4) found in the epidermis. These receptors activate transient receptor potential channels when stimulated, which causes calcium influx that sets off cellular responses.
Difference between blue light and red light in PDT
Doctors employ both lights in photodynamic therapy, but they work differently. Blue light (417 nm) stays closer to the surface compared to red light (630-635 nm), which goes deeper into skin layers. Studies showed that blue light PDT reached slightly higher clearance rates (98%) than red light PDT (93%) when treating skin cancer.
Patient comfort makes another big difference—blue light PDT hurts less during treatment. The reduced pain likely comes from blue light’s lower fluence rate (10 mW/cm² delivering 10 J/cm² over 1000 seconds) compared to red light’s higher intensity (75 mW/cm² delivering 37 J/cm² over 8 minutes). Gentle application of blue light over a longer time seems to cause less stimulation of PpIX-loaded nerve fibers.
Blue light PDT keeps Langerhans cell counts stable after treatment, while red light PDT substantially decreases these important immunosurveillance cells by 75%. Research also shows no signs of DNA damage or early photodamage after short-term blue light use, which confirms its safety for dermatological treatments.
FDA-approved uses for blue light therapy
FDA has cleared several ways to use blue light therapy in dermatology:
- Acne treatment – Blue light kills Propionibacterium acnes bacteria by exciting bacterial porphyrins (coproporphyrin III and protoporphyrin IX). FDA has approved 35 light-emitting diode (LED) devices to manage acne since 2009.
- Actinic keratosis treatment – FDA approved LEVULAN KERASTICK with BLU-U Blue Light Photodynamic Therapy to treat minimally to moderately thick actinic keratoses on the face, scalp, or arms.
- Psoriasis management – A wearable, UV-free blue light device helps treat mild psoriasis at home with FDA approval. This approach doesn’t cause skin cancer or premature aging signs like UV therapies.
- Precancerous and cancerous skin lesions – Blue light PDT effectively prevents skin cancer and removes precancerous and cancerous skin lesions that haven’t spread, with FDA approval.
Research continues to explore how blue light might help with eczema, hair loss, rosacea, and wound healing, beyond these proven uses.
Clinical Trial Results: 94% Success Rate Explained
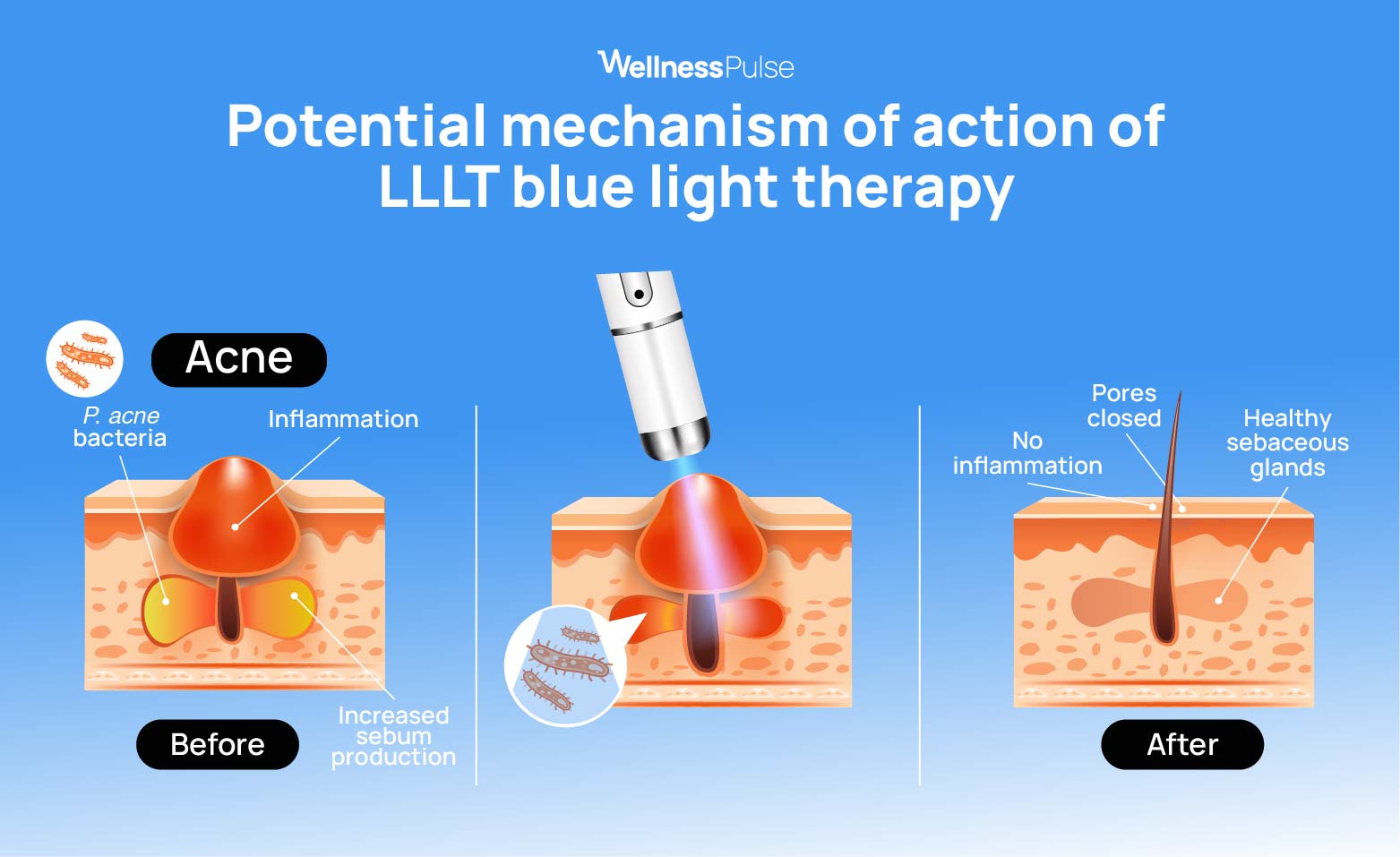
Image Source: WellnessPulse
Blue light therapy shows exceptional success rates in treating basal cell carcinoma (BCC). These clinical trials offer new hope to patients looking for alternatives to surgery.
Study design: Blue vs Red light in BCC patients
A groundbreaking pilot study showed how blue and red light photodynamic therapy (PDT) worked on the same patients. This gave researchers direct comparison data. The team recruited three patients with Basal Cell Nevus Syndrome (BCNS), also known as Gorlin syndrome. These patients had 141 BCC lesions. The study used a simple yet complete design. The team applied 5-aminolevulinate (20% solution) to all tumors. After 4 hours, half the tumors received blue light treatment while the rest got red light.
The team used an escalating light dose protocol over three biweekly treatment sessions across 4 months. This was to ensure patient safety. The blue light source (Blu-U) emitted at 417 nm with a power density of 10 mW/cm². It delivered a fluence of 10 J/cm² over 1000 seconds. The red light source (Aktilite CL128) worked at 630 nm with about 75 mW/cm² power density. It delivered 37 J/cm² in roughly 8 minutes.
Tumor clearance rates after 6 sessions
The original treatment cycle with lowest light fluence cleared very few tumors. The second cycle with intermediate fluence saw one-third to one-half of the tumors respond. The third cycle at highest fluence brought the most impressive results. Almost all tumors cleared.
Blue light therapy achieved a remarkable 98% clearance rate. This is a big deal as it means that red light’s 93% success rate. Statistical analysis confirmed blue light PDT matched red light PDT with a confidence level of p<0.001. The treatment works as well as or better than many traditional approaches.
Pain levels and patient satisfaction comparison
Blue light therapy proved more comfortable for patients. They reported less pain during blue light sessions compared to red light treatments. This matters because PDT pain can be so severe that some patients stop treatment or avoid future sessions.
The patients rated both treatments very favorably at the study’s end. They noticed no major difference in side effects between blue and red light.
Histological confirmation of treatment success
The final evaluation at 6 months included biopsies of suspicious lesions to confirm results. Eight lesions underwent biopsy, and six showed positive for BCC. Red light treated five of these persistent tumors, while blue light treated only one. This further proves blue light’s effectiveness.
This direct comparison shows that blue light PDT matches and might even work better than red light PDT for BCC treatment. Patients also find it more comfortable.
Treatment Process: From Photosensitizer to Light Exposure
Image Source: MDPI
PDT process needs careful application of photosensitizers and light exposure to target cancer cells. Each step of this process helps explain why clinical settings show such impressive success rates.
Use of 5-aminolevulinic acid (ALA) in PDT
ALA is the life-blood of modern PDT treatments. Unlike direct photosensitizers, ALA works as a precursor that builds up mostly in dysplastic cells. The cells absorb this compound and convert it to protoporphyrin IX (PpIX) through the heme biosynthesis pathway. This conversion happens mostly in abnormal cells’ mitochondria.
What makes this mechanism elegant is its selective nature. ALA gets into all cells but builds up by a lot more in tumor cells. Cancer cells show higher activity of enzymes that make PpIX, and they have less ferrochelatase activity that would normally turn PpIX into heme. These biochemical differences create perfect conditions to target therapy without harming healthy tissue.
Incubation period and light exposure duration
Old protocols needed long 1-3 hour incubation periods after applying ALA. Doctors thought this waiting time was needed to let enough PpIX build up to work. Recent studies have showed similar results with shorter waiting times.
Standard treatments now need 30 minutes to 2 hours before blue light exposure. The treatment area and condition severity determine the exact time needed. After this wait, blue light exposure takes exactly 16 minutes and 40 seconds, though protocols can vary.
Some new approaches have looked at immediate light exposure without waiting periods. These methods make up for it with longer light exposure times. Light exposure duration might matter more than incubation time.
Fluence levels: 10 J/cm² to 20 J/cm² for blue light
Blue light therapy needs proper energy adjustment to get the best results. Standard protocols start with 10 J/cm² fluences – the energy density given to the treatment area.
Doctors might increase the fluence for tough or resistant lesions by extending light exposure time. Clinical trials have showed that increasing protocols up to 20 J/cm² for blue light is safe and works well. They achieve this by extending light exposure time by about 50% in later treatments.
Red light treatments use much higher fluence levels of 37-75 J/cm² at higher power densities. This explains in part why blue light treatments cause less discomfort but work just as well or better.
Post-Treatment Recovery and Side Effects
Image Source: Nature
Blue light therapy for skin cancer leads to predictable recovery patterns that need specific care. Proper management of these effects will lead to better healing and treatment results.
Common reactions: redness, peeling, and swelling
Most patients show a consistent recovery pattern after blue light skin treatment. The treated area becomes red, swollen, tender, and sometimes shows mild bruising or blistering right after treatment. Patients notice redness or skin color changes on day 1, which get stronger on day 2. Itchy and peeling skin usually shows up between days 3-7, and some rare cases might develop blisters. Complete healing happens within 7 days for most people, but crusting can take anywhere from 3-14 days to clear up.
Photosensitivity precautions for 48 hours
The skin stays very sensitive to light for at least 48 hours after treatment, so you need strong protection from all light exposure. During this key period, patients should:
- Stay indoors, particularly in the first 48 hours
- Keep away from bright indoor lights and helmet-type hair dryers
- Use sun-protective clothing, wide-brimmed hats, and scarves if they must go outside
Regular sunscreens won’t protect enough against light sensitivity. However, doctors strongly recommend sunblock with zinc oxide or titanium dioxide every 2-3 hours as extra protection.
Pain management strategies during and after PDT
Pain is the biggest drawback of blue light therapy for skin cancer, and it can become intense or unbearable at times. Several strategies can help reduce discomfort. Cold pain relief, shots of local anesthetic, nerve blocks, and electrical nerve stimulation work well, but numbing gels usually don’t help much.
Over-the-counter medicines like acetaminophen, ibuprofen, or aspirin can help with pain after treatment. Antihistamines such as Benadryl can reduce itching and swelling. Many patients find quick relief by using ice packs or cold compresses.
Comparing Blue Light Therapy to Other Skin Cancer Treatments

Image Source: NCBI – NIH
Doctors must carefully evaluate the effectiveness of different skin cancer treatments. Blue light therapy is one of several options available among other treatments, and each has its own benefits.
Cryotherapy vs blue light therapy for actinic keratosis
Doctors have long used cryotherapy’s liquid nitrogen freezing as their go-to treatment for actinic keratoses. Research now shows that photodynamic therapy (PDT) gets better results. Blue light PDT gives patients a 14% better chance of completely clearing thin lesions on the face and scalp within 3 months compared to cryotherapy. Patients feel less pain with daylight PDT than with cryotherapy (mean VAS 0.9 vs 3.2). Cryotherapy leaves white marks after healing, but PDT gives excellent cosmetic results with minimal scarring.
Topical chemotherapy vs PDT: inflammation and coverage
Topical treatments like 5-fluorouracil (5-FU) work well against actinic keratoses but cause a lot of inflammation. Studies show 5-FU is slightly more effective than ALA-PDT, which makes it a better choice for treating large areas. In spite of that, patients need to apply topical chemotherapy daily for several weeks. This leads to long healing periods with irritation, redness, and crusting. Blue light therapy for skin needs fewer office visits and has shorter recovery times. This makes it a better option for patients who want convenience over longer treatment periods.
Surgical excision vs PDT: scarring and recurrence
Surgical excision remains the best way to treat basal cell carcinoma. Five-year studies show that excision keeps a 96% clearance rate compared to PDT’s 76%. The recurrence rate after surgery is still 4% versus 14% with PDT. Blue light treatment’s biggest advantage lies in its cosmetic results, especially on the face. PDT leaves minimal scarring and preserves skin texture better. Yes, it is clear that patients are much happier with how they look after PDT compared to surgery, which can leave scars and uneven contours.
Conclusion
Blue light therapy is a breakthrough in skin cancer treatment that gives patients a non-surgical option with amazing results. The numbers tell the story – it clears 98% of basal cell carcinomas, beating red light therapy’s 93% success rate. This treatment works great for patients who want minimal scarring, especially when you have facial lesions.
Patients feel way less pain with blue light therapy than red light options, so they stick with the treatment and feel better about it. The process uses special light-sensitive materials that target cancer cells while leaving healthy tissue alone. Some side effects like redness, swelling, and peeling show up but go away within a week – that’s a pretty quick recovery.
Blue light therapy beats traditional treatments in several ways. Unlike cryotherapy that leaves permanent white marks, it keeps your skin looking natural. Surgery works but always leaves scars – something blue light therapy mostly avoids. Regular chemotherapy needs daily treatment for weeks, while blue light needs fewer sessions, making life easier for patients.
The FDA has backed blue light therapy beyond just treating skin cancer. They’ve approved it to treat acne, psoriasis, and actinic keratosis too. This flexibility, plus its great success rate, makes it a powerful weapon against skin cancer in modern dermatology.
This treatment gives new hope to patients dealing with multiple or recurring lesions. It works well and helps maintain their quality of life. What a world of blue light therapy looks bright as scientists keep improving it and finding new ways to use this promising treatment.
FAQs
Q1. How effective is blue light therapy for treating skin cancer?
Blue light therapy has shown remarkable effectiveness in treating certain types of skin cancer, particularly basal cell carcinoma. Recent clinical trials have demonstrated a 98% clearance rate for basal cell carcinoma lesions, slightly outperforming red light therapy’s 93% success rate.
Q2. What are the advantages of blue light therapy over other skin cancer treatments?
Blue light therapy offers several advantages, including minimal scarring, shorter recovery times, and less pain during treatment compared to options like surgery or cryotherapy. It’s particularly beneficial for facial lesions where cosmetic outcomes are important. Additionally, it requires fewer treatment sessions than topical chemotherapy.
Q3. What should patients expect during the recovery period after blue light therapy?
After blue light therapy, patients typically experience redness, swelling, and tenderness in the treated area. Peeling and itching may occur between days 3-7. Most patients fully heal within 7 days, although some crusting may take up to 14 days to resolve completely. It’s crucial to protect the treated area from light exposure for at least 48 hours post-treatment.
Q4. Is blue light therapy FDA-approved for skin conditions other than cancer?
Yes, the FDA has approved blue light therapy for several dermatological applications beyond skin cancer treatment. These include acne management, treatment of actinic keratosis, and psoriasis management. Its versatility makes it a valuable tool in modern dermatology.
Q5. How does blue light therapy compare to red light therapy for skin cancer treatment?
While both are effective, blue light therapy has shown slightly higher clearance rates (98%) compared to red light therapy (93%) in treating basal cell carcinoma. Blue light also causes less pain during treatment and penetrates more superficially, making it particularly suitable for treating surface-level skin cancers and precancerous lesions.



