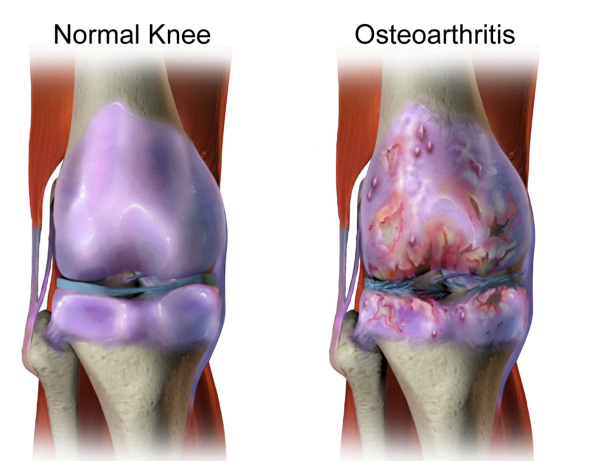
Knee osteoarthritis (OA) is a type of joint degeneration caused by wear and tear, resulting in
the gradual loss of articular cartilage and the subsequent rubbing of the bones together. This
rubbing causes pain, stiffness, and swelling. The knee bears great stress throughout daily
life because it is one of the most often affected joints.
The cause of osteoarthritis in the knee determines whether it is primary or secondary. Unknown causes of articular cartilage deterioration lead to primary osteoarthritis in the knee. Usually, this happens due to aging and wear and tear.
On the other hand, secondary osteoarthritis can be caused by either increased joint
pressure, as in post-traumatic injuries, or distorted articular cartilage, as in rheumatoid
arthritis (RA). Osteoarthritis affects the hands, hips, and spine in addition to the knees. The
intensity of symptoms varies from person to person and usually appears slowly.
Osteoarthritis affects the hands, hips, and spine in addition to the knees. The intensity of
symptom varies from person to person and usually appear slowly.
Relevant Anatomy about Physiotherapy for Knee
The knee joint is the largest joint in your body. This hinge-type synovial joint facilitates
standing, moving, and maintaining balance by allowing flexion and extension (as well as a
minor amount of medial and lateral rotation). Additionally, your knees have ligaments like
your LCL, MCL, ACL, and PCL, as well as cartilage like the meniscus.
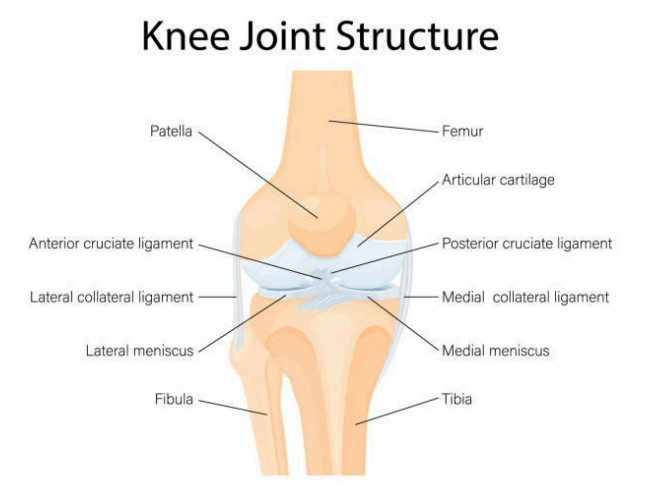
The knee joint has two articulations – tibiofemoral and patellofemoral
Tibiofemoral: The lateral and medial condyles of the femur articulate with the condyles of
the tibia. It is the weight-bearing portion of the knee joint.
Patellofemoral: By articulating with the patella, the anterior aspect of the distal femur
increases the muscle’s efficiency.
Stages of knee osteoarthritis
Although osteoarthritis in the knee doesn’t have defined stages, it is a degenerative disease
that develops gradually. (This type of arthritis is relatively different.) But it can help you better
understand your symptoms and what to plan for treatment next.
Stage 1 (Minor): Indicates that your knee joint’s cartilage is starting to degrade. Most likely,
you haven’t experienced any pain yet.
Stage 2 (Mild): Your knee joint may begin to feel stiff and painful during the mild stage, but
there is still enough cartilage to prevent the bones from rubbing against one another.
Stage 3 (Moderate): In this stage, cartilage has drastically decreased. It puts more pressure
on the knees, specifically in walking, bending, kneeling, and jogging. Additionally, you may
experience more pain and joint stiffness after long hours of inactivity.
Stage 4 (Severe): Your knee’s cartilage is nearly gone in this stage, which causes the bones
to rub against one another during activity. You have pain, stiffness, and immobility in your
knee. You may now think about having knee replacement surgery.
Some typical clinical signs are
● Slow-onset, intermittent, or persistent knee pain that gets worse with movement
● Morning swelling and stiffness that lasts less than half an hour
● Pain after long sitting
● Crepitus or a cracking sound during activity
● Knee locking or giving way
● Inability to move, climb stairs, or carry out household tasks
Epidemiology
The most common type of arthritis is knee osteoarthritis, and
it’s frequency will continue to increase as the quality of life and
overweight. Moreover, it is seen in some research about 10%
of men and 13% of women aged 60 and above have
symptomatic osteoarthritis in their knees. The frequency
increases to as much as 40% among people over 70.
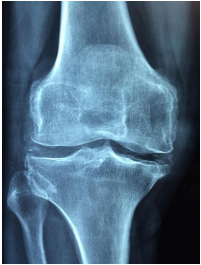
In addition, men are less likely than women to get knee
osteoarthritis. It’s important to note that not all patients with
knee osteoarthritis have symptoms on radiographs. According
to one study, only 15% of patients with knee OA radiographic
results had any symptoms. Without accounting for age, there
are about 240 incidences of symptomatic knee osteoarthritis
for every 100,000 people annually.
Pathophysiology
The main constituents of articular cartilage are water, chondrocytes, proteoglycans, and type
II collagen. The components of healthy articular cartilage are always in balance with one
another, allowing any cartilage deterioration to be compensated for. Therefore, articular
cartilage remains healthy.
During osteoarthritis, the overproduction of matrix metalloproteases (MMPs), or degradative
enzymes, disturbs the balance and causes a loss of collagen and proteoglycans. However, i
n the early stages of osteoarthritis, chondrocytes release tissue inhibitors of MMPs (TIMPs)
and aim to speed up the synthesis of proteoglycans to accommodate the degradative
activity. But this process of reparation is insufficient.
Even though there is more synthesis, more water, a messy pattern of collagen, and
eventually less articular cartilage elasticity, the loss of balance leads to a drop in the number
of proteoglycans. These alterations cause the cartilage to weaken and tear on a
macroscopic level, which eventually leads to the deterioration of the articular surface.
Since there is a strong correlation between knee osteoarthritis and age, it is crucial to
remember that knee osteoarthritis is a disease in and of itself rather than just a result of
aging. It can be verified by the changes seen in cartilage with both osteoarthritis and aging.
In addition, the enzymes that break down cartilage function at normal levels in healthy aging
cartilage, but in knee osteoarthritis, they are produced in greater quantities.
Risk factors
The following factors may increase your risk of knee OA:
● If the body mass index (BMI) is 30 or more
● Any history of knee injury
● Overstress your knee when playing sports or at work.
● Family history of knee osteoarthritis.
● Uneven joints or bones, like “knock knees.”
Differential Diagnosis
● Meniscal pathology
● Patellofemoral pain syndrome
● Gout and Pseudogout
● Rheumatoid arthritis
● Septic arthritis
● Hip OA
● Referred lower back pain
● Ligament injury, ACL or PCL rupture
Management/Treatment
There are two types of treatment for knee OA: conservative and surgical.
However, physical therapy and patient education are the first-line treatments for all patients
with symptomatic knee osteoarthritis. It has been found that the best outcomes come from a
combination of at-home exercise and supervised exercise. The results are lost after 6
months if the exercises are discontinued. It is a tested intervention by the American
Academy of Orthopedic Surgeons (AAOS).
Conclusion
Initially, conservative treatment is the most effective way to address knee OA. If this strategy
fails and there is positive radiographic evidence of OA, surgical treatments may be done to
enhance the quality of life and relieve pain.
Since there is no known cure for OA, different approaches help to stop the progression of
the condition. A holistic approach (i.e. physiotherapist, dietitian and pharmacist) is required to
promote good health and manage pain. Lastly, if pain becomes unbearable, it is crucial to
consult orthopaedic specialists.