Small cell lung cancer ranks among the deadliest forms of cancer. Patients rarely live beyond a few months without proper treatment. The numbers paint a grim picture – patients with limited disease SCLC live only 15-20 months (median survival), while five-year survival rates stay between 10-13%. The situation becomes more dire for extensive small cell lung cancer patients. This group makes up about 70% of all cases, with survival rates dropping to 8–13 months and five-year survival plummeting to just 1%–5%.
These statistics seem overwhelming, yet one person’s remarkable trip shows that small cell lung cancer might be beatable. Most patients lose their battle within months of diagnosis, but some extraordinary cases demonstrate the possibility of victory over this aggressive disease. A small number of patients beat their original cancer, and their stories are a great way to get hope and inspiration for others battling this diagnosis.
This piece shares details from what researchers consider one of the longest documented cases of extensive-stage small cell lung cancer survival. The patient received cutting-edge treatments that combined CIK immune cell therapy with chemotherapy. Their story shows that extended survival and better quality of life are possible even with one of cancer medicine’s toughest challenges.
Facing the Diagnosis: What It Means to Hear ‘Small Cell Lung Cancer’

A small cell lung cancer (SCLC) diagnosis changes life in a heartbeat. The sudden move from normal life to uncertainty leaves patients and families dealing with mixed emotions and questions about the future.
Understanding the prognosis and survival rates
The numbers for SCLC paint a serious picture. Recent data shows the overall 5-year relative survival rate for all SCLC stages combined stands at about 9%. Doctors often explain survival rates based on how far the cancer has spread:
- Localized disease (confined to one area): 34% five-year survival rate
- Regional spread (to nearby structures): 20% five-year survival rate
- Distant spread (to other body parts): 4% five-year survival rate
Median survival times tell us when half of patients are still alive. Limited stage SCLC patients live 12 to 16 months with treatment. Extensive stage SCLC patients live 7 to 11 months with treatment.
These numbers represent averages from large patient groups. Each person’s outcome can differ by a lot based on their age, health, genetic markers, and response to treatment. The statistics come from patients diagnosed years ago, and new treatments continue to improve outcomes.
Is small cell lung cancer curable?
The simple answer is yes—with some important details. Limited stage disease offers a cure to about 20-25% of people. About 25% of people with limited stage SCLC can beat the disease with early treatment that combines chemotherapy and radiation therapy.
Extensive stage disease presents bigger challenges. Though extensive stage SCLC has no cure yet, treatments can shrink tumors, ease symptoms, keep quality of life high, and help people live longer. SCLC grows faster without treatment, and patients live only 2 to 4 months after diagnosis.
Clinical trials bring fresh hope as scientists study targeted therapies and new approaches. About 10% of SCLC patients stay cancer-free for 2 years after starting treatment. This number might look small but represents thousands of people who beat the odds.
How this survivor processed the news
Real survival stories give us hope beyond statistics. Marianne’s story stands out. Doctors gave this 41-year-old mother a 5% chance to live. She thought about her young daughter and spent her “limited” time making special memories. Today, 13 years later, she still creates those memories.
“Your personal cancer story cannot be defined by statistics or predictions,” Marianne tells other patients.
Matt’s story inspires too. His doctor thought he wouldn’t survive treatment after finding extensive disease. Two years later, Matt proves those predictions wrong. He suggests learning all you can about SCLC, getting second opinions, and focusing on living with cancer rather than just fighting it.
Lindy found her strength through a clinical trial and faith. She stresses how important it is to know what treatment brings and stay open to experimental options.
These stories show a vital truth: you might face SCLC with grief, anger, numbness, or determination—but hope remains your companion on this experience ahead.
The Treatment Journey: From Standard Protocols to Personalized Care

The battle against small cell lung cancer starts with proven treatment protocols. Your journey to becoming a long-term survivor might need tailored adjustments as you progress.
Original chemotherapy and radiation
A combination of chemotherapy and radiation therapy forms the backbone of small cell lung cancer treatment. Patients with limited-stage disease receive platinum (cisplatin or carboplatin) with etoposide as the most accessible chemotherapy regimen. This protocol combined with thoracic radiation therapy has helped patients achieve median survivals of 18 to 24 months and 2-year survival rates of 40% to 50%.
The timing of radiation therapy is vital to treatment success. Several clinical trials point to small benefits when radiation therapy starts during the first or second cycle of chemotherapy. This combined approach, called chemoradiation, shows a modest but significant 5% improvement in 3-year survival rates compared to using chemotherapy alone.
Doctors treat extensive-stage disease with chemotherapy alone or combine it with immunotherapy drugs like atezolizumab (Tecentriq) or durvalumab (Imfinzi). These medications continue as maintenance therapy after the original treatment phase.
Adjusting treatment based on side effects
Side effects often lead to necessary treatment adjustments. Chemotherapy commonly causes fatigue, nausea, hair loss, and weakened immunity. Radiation therapy can lead to skin changes, tiredness, and swallowing difficulties.
Managing these side effects becomes just as important as curbing the cancer. Your doctor might:
- Give you anti-nausea medications to ease digestive problems
- Change your treatment schedule to help you recover
- Show you ways to stay hydrated and flush out toxins
- Recommend light exercise to fight fatigue
Some patients with poor health might need lower doses of chemotherapy or focus on palliative care. Targeted radiation therapy or other localized treatments help relieve severe symptoms like shortness of breath when cancer grows in the lungs.
Learning about alternative therapies like cryoablation
Cryoablation stands out as a promising option beyond standard treatments. This minimally invasive procedure freezes cancer cells to destroy them. Doctors insert a needle-like applicator called a cryoprobe through a tiny puncture and deliver very cold gas (like liquid nitrogen or argon) straight to the tumor.
Cryoablation benefits patients with early-stage tumors or those who can’t have surgery. The procedure:
- Needs no incision
- Creates minimal scarring with fewer side effects
- Protects nearby tissues from damage
This technique works well to control lung cancers locally. It destroys tumor cells and might boost your body’s immune response by releasing antigens.
Research shows lung ablation controls early-stage lung cancer or limited metastatic disease effectively. Some patients showed 96% recurrence-free survival at 3 years after treating tumors smaller than 2cm.
The Role of Immunotherapy in Long-Term Survival
Immunotherapy brings new hope to patients who want to beat small cell lung cancer and live longer. Standard treatments often reach their limits, but immune-based approaches create fresh possibilities to fight this aggressive disease.
What is CIK cell therapy?
Cytokine-induced killer (CIK) cells provide a powerful immunotherapy option. These specialized cells consist of T cells with natural killer-like abilities, expanded from a patient’s own peripheral blood mononuclear cells. The process starts with cell collection, followed by stimulation with multiple cytokines including interferon-gamma, anti-CD3 monoclonal antibody, and interleukin-2 for 14-21 days. Doctors then reinfuse these cells back into the patient’s body.
CIK cells fight cancer through several methods. They kill tumor cells directly by releasing granzyme and perforin. These cells also produce various cytokines that inhibit tumors and regulate immune responses. Their ability to target and move toward tumors and tumor-associated tissues makes them even more effective at fighting cancer.
Combining immune cells with chemotherapy
CIK therapy works best when combined with standard chemotherapy. Research shows chemotherapy can boost the anti-tumor effects of immune cells. This happens as CD8+ T memory cells transform into CD8+ T effector cells and more immune cells penetrate the tumor environment.
This collaborative effort offers key benefits:
- CIK cells destroy tumor cells that resist chemotherapy
- Combined treatments overcome drug resistance better than chemotherapy alone
- The treatment sequence (chemotherapy followed by CIK therapy) delivers optimal results
Clinical studies validate this approach. One trial revealed that patients who received CIK cells with chemotherapy achieved an impressive 82.4% objective response rate and 100% disease control rate.
Tracking immune markers like CD4/CD8 ratio
Many patients ask “has anyone beat small cell lung cancer?” The answer lies in tracking specific immune markers to learn about treatment success. The CD4/CD8 ratio emerges as a crucial metric. This ratio shows the balance between different T cells and reveals the body’s immune status.
Research identifies 1.93 as a key CD4/CD8 threshold. Patients with ratios above 1.93 showed substantially better outcomes. Their median progression-free survival reached 18.4 months compared to 1.2 months for those with lower ratios. Higher CD4/CD8 ratios relate to better overall survival rates, making this an essential measurement.
Doctors use these immune markers to guide treatment decisions for small cell lung cancer survivors. The answer to “is small cell lung cancer curable?” depends on how well we can control the body’s immune system to fight the disease.
Monitoring Progress: How Stability Was Maintained Over the Years
Small cell lung cancer patients need both effective treatment and careful monitoring to survive long-term.
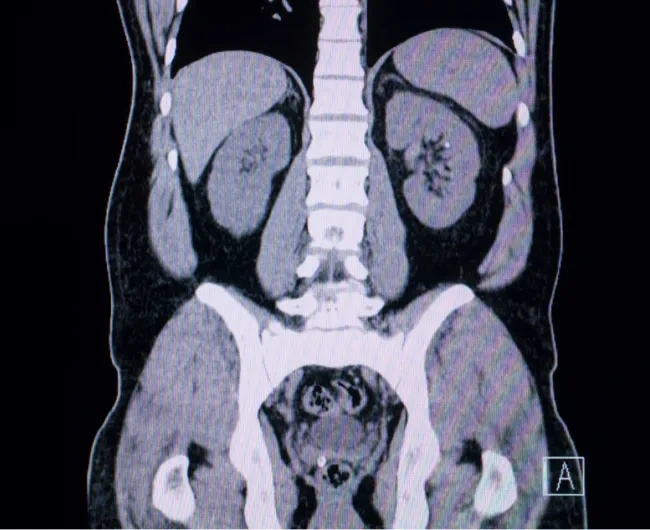
CT scans and blood tests track progress
The life-blood of care for long-term survivors lies in careful monitoring. CT scans work better than regular chest x-rays to create detailed cross-sectional images that detect tumors. These scans show the exact size, shape, and location of lung tumors and can spot enlarged lymph nodes containing cancer.
Blood tests that track specific tumor markers are a great way to get information about disease activity. Markers like neuron-specific enolase (NSE) and pro-gastrin-releasing peptide (Pro-GRP) often increase when the disease becomes active. Higher levels can signal the cancer growing. One case showed elevated markers before doctors found enlarged lymph nodes.
Better life quality through side effect control
Quality of life plays a vital role throughout this process. Common challenges include:
- Fatigue affects about 90% of survivors
- Early-stage survivors often deal with breathing problems and cough, seen in up to 60% of cases
- Pain after treatment can lead to depression and poor sleep
Good management needs targeted approaches. Patients who ask for palliative care focused on symptom control (not end-of-life care) often do better. This approach helps patients live longer and function better daily.
Understanding dormant tumors
Tumor dormancy brings hope as cancer cells exist without showing clinical signs of growth. Dormant cancer cells typically show:
- Cell cycle stops at G0/G1 phase that can reverse
- Minimal cell death and treatment resistance
- Slower cell metabolism
This explains why some patients stay disease-free for extended periods after treatment. Dormant cells might hide for years or decades before becoming active again. Understanding how dormancy works gives us a new point of view on beating small cell lung cancer. Sometimes managing the disease, rather than eliminating it completely, helps patients become long-term survivors.
Lessons from the Longest Survivor: What We Can Learn

Small cell lung cancer survivors teach powerful lessons to patients, caregivers, and medical professionals.
Has anyone beat small cell lung cancer? Yes.
Success stories shine brightly. Maida Mangiameli’s story stands out – she’s been in remission for six years and continues to inspire others with her strength. Her experience shows how patients can live longer than expected, even with what many would call a terminal diagnosis. Some patients have lived almost 15 years after getting diagnosed with stage 4 lung cancer. These survivors prove you can beat the odds.
The importance of early immune assessment
Your immune markers can make a big difference in treatment success. Research shows better outcomes for patients with CD4/CD8 ratios above 1.93. This is a big deal as it means that their progression-free survival reached 18.4 months compared to just 1.2 months for those with lower ratios. Early CT screening is a vital part too – 80% of patients who catch lung cancer early live 20 years or more.
Hope, resilience, and the future of treatment
Mental strength plays a key role in this experience. Research shows hope helps people cope better with cancer, improves wellbeing, and reduces anxiety and depression. We have more reasons to stay positive:
- TIL therapy (tumor-infiltrating lymphocytes) works well for some SCLC patients
- New immunotherapy drugs like tarlatamab target specific proteins on SCLC cells
- Treatment combinations show promising results
Each survivor reminds us that statistics tell group stories, not individual ones.
Conclusion
This piece explores the incredible stories of people who beat the odds in their fight against small cell lung cancer. The statistics paint a grim picture, but these stories show that living longer is possible. Take Marianne, who has survived 13 years after her diagnosis. Her case proves patient outcomes can vary significantly from average statistics.
Long-term survivors often combine traditional treatments with new approaches. While chemotherapy and radiation therapy are the foundations of treatment, adding immunotherapies like CIK cell treatment shows great promise. This multi-pronged strategy tackles cancer from different angles and helps overcome resistance to single treatments.
CT scans and tumor marker monitoring have proven vital for patients who stayed stable over the years. The ability to manage side effects helps maintain a good quality of life—which affects long-term outcomes. Tumor dormancy explains why some patients enjoy extended periods without disease after treatment.
These survival stories demonstrate the power of hope. A small cell lung cancer diagnosis is serious, but hope does more than comfort—it motivates patients to try new treatments, join clinical trials, and fight beyond statistical predictions.
New treatments like TIL therapy and immunotherapy drugs give more reasons to be optimistic. These advances, combined with better understanding of immune markers and individual-specific treatment approaches, improve patient outlook steadily.
“Has anyone beat small cell lung cancer?” The answer is yes. The road ahead remains tough, but these survivors prove statistics reflect populations, not individuals. Their experiences show that with proper treatment, careful monitoring, and steadfast dedication, patients can achieve longer survival and better life quality—even against one of cancer’s toughest diagnoses.
Key Takeaways
While small cell lung cancer has challenging statistics, remarkable survival stories prove that beating this diagnosis is possible with the right approach and mindset.
• Long-term survival is achievable: Patients like Marianne have lived 13+ years beyond diagnosis, proving statistics don’t define individual outcomes.
• Combined treatments show promise: Integrating standard chemotherapy with innovative immunotherapies like CIK cell therapy dramatically improves response rates to 82.4%.
• Immune monitoring guides success: Patients with CD4/CD8 ratios above 1.93 achieve 18.4 months median survival versus just 1.2 months for lower ratios.
• Early detection saves lives: 80% of early-stage lung cancer patients live 20+ years, emphasizing the critical importance of screening and prompt treatment.
• Hope drives better outcomes: Psychological resilience correlates with enhanced well-being, lower anxiety, and improved coping—making hope a powerful treatment ally.
The journey may be difficult, but these longest survivors demonstrate that with personalized care, vigilant monitoring, and unwavering determination, extended survival and quality of life remain within reach even for this aggressive cancer type.
FAQs
Q1. Is it possible to survive small cell lung cancer?
Yes, it is possible to survive small cell lung cancer. While the overall prognosis can be challenging, there are documented cases of long-term survivors. For instance, some patients have lived nearly 15 years after a stage 4 lung cancer diagnosis. Early detection, personalized treatment approaches, and advances in immunotherapy have improved survival rates for some patients.
Q2. What are the latest treatment options for small cell lung cancer?
Recent advancements in small cell lung cancer treatment include immunotherapy drugs like atezolizumab and durvalumab, often used in combination with chemotherapy. Additionally, innovative approaches such as CIK (Cytokine-induced killer) cell therapy and TIL (tumor-infiltrating lymphocytes) therapy are showing promise. Targeted therapies like tarlatamab, which specifically target proteins found on SCLC cells, are also being developed.
Q3. How important is immune system monitoring in SCLC treatment?
Immune system monitoring plays a crucial role in SCLC treatment. Tracking markers like the CD4/CD8 ratio can significantly impact treatment outcomes. Research shows that patients with CD4/CD8 ratios above 1.93 experienced dramatically better outcomes, with median progression-free survival of 18.4 months compared to just 1.2 months for those with lower ratios.
Q4. Can small cell lung cancer go into remission?
Yes, small cell lung cancer can go into remission. While it’s considered a challenging cancer to treat, some patients achieve remission through aggressive treatment. For example, there are cases like Maida Mangiameli, who has been in remission for six years. The concept of tumor dormancy also explains how some patients can experience extended disease-free periods after treatment.
Q5. How does maintaining quality of life impact SCLC survival?
Maintaining quality of life is crucial for SCLC survival. Managing side effects effectively, addressing symptoms like fatigue and pain, and focusing on overall well-being can positively impact treatment outcomes. Studies have shown that patients who receive palliative care focused on symptom management alongside their cancer treatment not only have better quality of life but may also live longer.





