Overview of the Diabetes honeymoon phase.
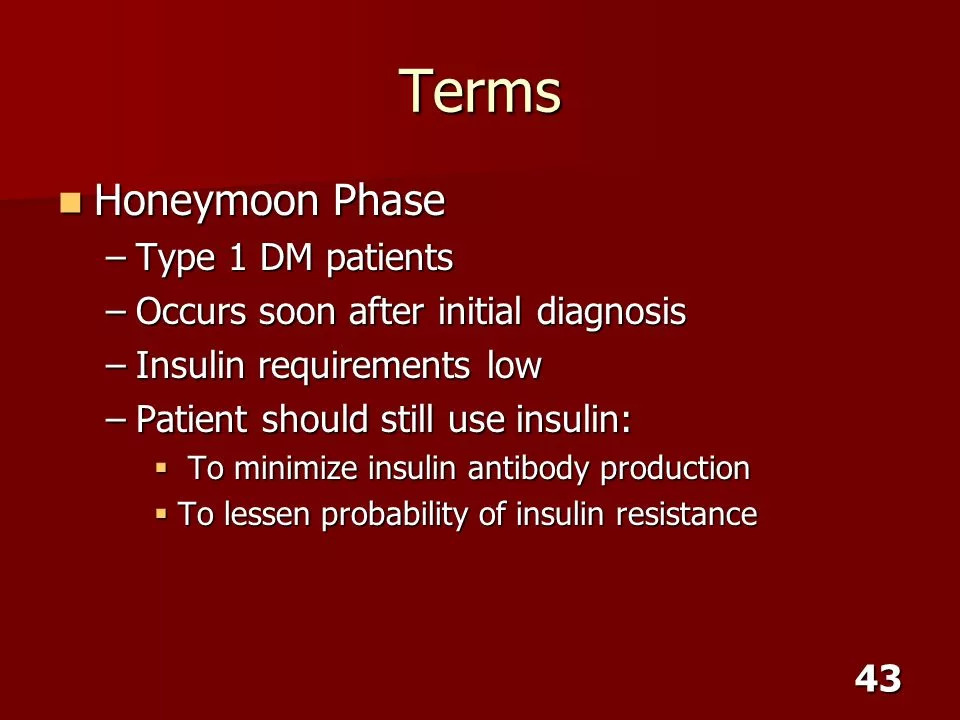
The “Diabetes honeymoon phase” refers to a period of time after the initial diagnosis of type 1 diabetes when the pancreas can still produce some insulin.During this phase, individuals may require less insulin or may even appear to have normal or near-normal blood glucose levels without the need for insulin.
However, this phase is usually temporary, and eventually, the pancreas’s ability to produce insulin decreases further, requiring the individual to return to regular insulin treatment.This phase can vary in duration, with some individuals experiencing it for a few months, while others may have it for up to a year or more.
It’s important for people experiencing this phase to work closely with their healthcare team to monitor their blood sugar levels and adjust their treatment plan accordingly.
What is the significance of the “diabetes honeymoon phase” for individuals diagnosed with type 1 diabetes in terms of insulin production and management strategies?
Upon receiving a diagnosis of type 1 diabetes, individuals may experience what is commonly referred to as the “diabetes honeymoon phase.”
This phase represents a temporary period during which the pancreas continues to produce some insulin, leading to a decreased need for exogenous insulin. Understanding the dynamics, challenges, and management strategies during this phase is crucial for both patients and healthcare providers.
What is the Diabetes Honeymoon Phase?
The Diabetes honeymoon phase, typically occurring after the initial diagnosis of type 1 diabetes, involves a partial restoration of beta-cell function within the pancreas. As a result, the individual’s insulin requirements may temporarily decrease, and their blood sugar levels may stabilize without the need for additional insulin.
This respite, however, is transitory, as the pancreas’s insulin production eventually declines further, necessitating a return to regular insulin therapy.
Duration and Variability:
The duration of the honeymoon phase can vary significantly among individuals.While some may experience this phase for a few months, others might enjoy its benefits for a year or more.
Understanding the individual variability in the duration of this phase is crucial for managing expectations and planning for future diabetes management.
Challenges and Considerations:
Despite the temporary relief provided by the honeymoon phase, it poses several challenges for both patients and healthcare professionals. Individuals may develop a false sense of security as their insulin requirements decrease, potentially leading to noncompliance with their treatment plans. Furthermore, the unpredictable nature of the phase can make it difficult for healthcare providers to determine the appropriate long-term treatment strategy.
Management Strategies:
Effectively managing the Diabetes honeymoon phase requires a comprehensive approach that emphasizes education, vigilance, and collaboration.
Patients should receive detailed education on the temporary nature of the phase and the importance of adhering to their treatment plans.Regular monitoring of blood glucose levels, coupled with close communication between patients and healthcare providers,is essential for making timely adjustments to the treatment regimen.
Long-Term Planning:
While the honeymoon phase provides a brief reprieve, it is essential for patients and healthcare professionals to plan for the eventual decline in pancreatic function. Developing a long-term management strategy that anticipates the progressive loss of endogenous insulin production is crucial for maintaining optimal blood glucose control and preventing complications associated with uncontrolled diabetes.
Below is more detail in simple words Certainly, here’s a complete guide on the Diabetes honeymoon phase.

Why and how diabetes occurs?
Diabetes occurs when the body has difficulty regulating the level of sugar (glucose) in the blood.
This can happen for two main reasons.In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
This results in little to no insulin production. In type 2 diabetes, the body either doesn’t produce enough insulin or becomes resistant to its effects, leading to an accumulation of glucose in the bloodstream.
Various factors, including genetics, lifestyle, and environmental factors, can contribute to the development of both types of diabetes.

How is insulin therapy administer?
Insulin therapy can be administered in various ways, including injections with a syringe, insulin pen, or an insulin pump.
The injections are typically administered into the fatty tissue, such as the abdomen, thighs, or upper arms. Insulin pens provide a convenient and discreet way to administer insulin, while insulin pumps deliver a continuous supply of insulin through a small tube inserted under the skin.
The method of administration may vary depending on the individual’s specific needs and preferences, as determined by their healthcare provider.
In diabetes Honey moon phase care and abstain
During the diabetic honeymoon phase, it’s crucial to closely monitor blood sugar levels and follow a well-balanced diet as prescribed by the healthcare provider. It’s essential to continue any recommended medications or insulin therapy.
Abstaining from excessive consumption of sugary foods and refined carbohydrates can help maintain stable blood sugar levels. Regular exercise and maintaining a healthy lifestyle are also important during this phase.
Additionally, maintaining open communication with a healthcare provider is crucial to managing this transitional period effectively.
How long does the Diabetic honeymoon period last?
The Diabetic honeymoon period, which occurs in some people with type 1 diabetes, can vary in duration. It typically lasts for a few weeks to a few months, but in some cases, it can last up to a year or more.
During this phase, there is a temporary improvement in insulin production, leading to a decrease in the need for external insulin. However, eventually, the pancreas function declines, and the individual will require insulin treatment as usual.
Complete diet plan Creating a complete diet plan would be best done with the guidance of a healthcare provider or a registered dietitian who can tailor the plan to your specific needs.
However, some general guidelines for a healthy diet plan for managing diabetes include:
- Incorporating a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limiting the intake of processed and high-fat foods.
- Monitoring carbohydrate intake and choosing complex carbohydrates over simple ones.
- Avoiding sugary beverages and foods high in added sugars.
- Spreading out meals throughout the day to maintain stable blood sugar levels.
- Paying attention to portion sizes and practicing mindful eating.
- Staying hydrated with water and avoiding sugary drinks.
Remember, individual dietary needs can vary, so it’s important to work with a healthcare professional to create a personalized plan that suits your specific health goals and lifestyle.

Which fruits and vegetables useful For individuals managing diabetes?
some fruits and vegetables can be particularly beneficial due to their low glycemic index and high fiber content.
Examples of fruits and vegetables that can be helpful include:
Fruits:
- Berries (such as strawberries, blueberries, raspberries)
- Apples
- Citrus fruits (like oranges and grapefruits)
- Pears
Vegetables:
- Leafy greens (like spinach, kale, and collard greens)
- Broccoli
- Carrots
- Bell peppers
These fruits and vegetables can be incorporated into a balanced diet to help manage blood sugar levels and provide essential nutrients.
However, portion control is still essential, and it’s crucial to consult a healthcare provider or a registered dietitian to determine the best choices based on individual dietary needs and preferences.
Conclusion:
The Diabetes honeymoon phase serves as a unique and temporary period for individuals with type 1 diabetes, during which their insulin requirements may temporarily decrease.
However, understanding the temporary nature of this phase, along with effective education and close monitoring, is crucial for ensuring a smooth transition to a long-term diabetes management plan that addresses the progressive decline in pancreatic function.
By staying informed and proactive, individuals and healthcare professionals can navigate the challenges posed by the Diabetes honeymoon phase and lay the foundation for effective long-term diabetes management. Add some more articles
What is Celiac disease? 100% Complete wheat Allergy Treatment





